[ad_1]
Federal regulators have abandoned a plan that physicians, patients and advocacy groups for breast cancer patients feared would limit women’s options for reconstructive surgery.
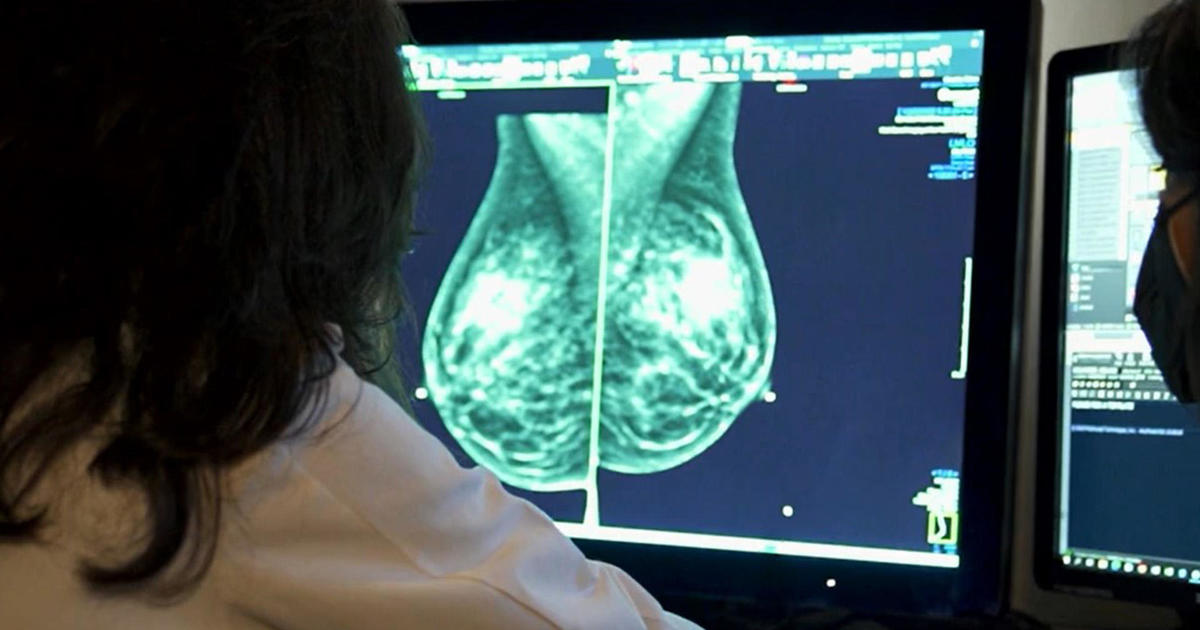
The controversy centered on how doctors are paid for a type of breast reconstruction known as DIEP flap, in which skin, fat and blood vessels are harvested from a woman’s abdomen to create a new breast.
Last year, the Centers for Medicare and Medicaid Services decided to eliminate a trio of medical billing codes for breast reconstructive surgery that enabled doctors to collect much more money for DIEP flap operations than for simpler types of breast reconstruction. Some plastic surgeons said the government’s move would limit access and make DIEP flaps available only to those who could afford to pay tens of thousands of dollars out of pocket.
Through its coding decisions, the federal government can influence the medical options available to patients, even those with private insurance.
In an Aug. 22 memo, CMS wrote that it received a “substantial number of responses” verbally and in writing asking regulators to keep the “S” billing codes that reimburse doctors more for the surgery. “The majority of the commenters feel their accessibility will be, or has already been, impacted by the decision to eliminate the S codes,” the agency wrote in reversing its earlier plan.
Supporters praised CMS’ latest action. “I’m so grateful to CMS for this decision that is really meaningful,” Elisabeth Potter, a plastic surgeon who specializes in DIEP flap surgeries, said in a social media post.
The agency’s announcement came after it convened a public hearing in June, during which several patients, physicians and representatives of breast cancer advocacy organizations implored CMS officials to scrap their original plan. Otherwise, they said, access to DIEP flap surgery would diminish.
The DIEP flap procedure has potential benefits over implants and operations that take muscle from the abdomen. For example, although implants are less costly and less time-intensive to perform, they generally need to be replaced every 10 years or so. But DIEP flap surgery is also more expensive. If patients go outside an insurance network for the operation, it can cost more than $50,000. A plastic surgeons’ group argued some in-network doctors would stop offering the surgery if insurers paid significantly less.
“This decision is monumental for breast cancer patients and breast reconstruction,” Christy Huling, who had a double mastectomy and DIEP flap surgery, said during CMS’ June 1 meeting. Through tears, Huling said she is an avid outdoors person and that her life would have changed “drastically” if she’d instead had reconstruction surgery that removed muscle from her abdomen. “This procedure has allowed me to continue to maintain my quality of life,” she said of DIEP flap.
The government’s initial plan was driven by the Blue Cross Blue Shield Association, a major lobbying organization for health insurance companies. In 2021, the group asked CMS to discontinue the three S codes, arguing they were no longer needed, according to a CMS document.
CMS initially decided the codes would expire at the end of 2024; however, even with the delayed effective date, physicians said, the decision was starting to hinder access to DIEP flap surgery and create anxiety for patients. At least two major insurance companies told doctors they would no longer reimburse them under the higher-paying codes.
A bipartisan group of lawmakers also protested, including Democrats Rep. Debbie Wasserman Schultz, of Florida, and Sen. Amy Klobuchar, of Minnesota, who have both had breast cancer and Republicans Rep. James Comer, of Kentucky and Sen. Marsha Blackburn, of Tennessee. “This latest CMS decision will provide women with more certainty, and help ensure fair and equitable access to their choice of breast reconstruction techniques,” Wasserman Schultz said in a statement following CMS’ change.
Codes don’t dictate the amounts private insurers pay for medical services; those reimbursements are generally worked out between insurance companies and medical providers. However, using the targeted S codes, doctors and hospitals have been able to distinguish DIEP flap surgeries, which require complex microsurgical skills, from other forms of breast reconstruction that take less time to perform and generally yield lower insurance reimbursements.
CMS’ initial plan would have made it “impossible to continue doing high-volume, high-quality complex breast microsurgery for breast cancer patients,” Dhivya Srinivasa, a plastic surgeon in California who specializes in breast reconstruction, said during CMS’ June 1 hearing. “I am already seeing it, patients who are good candidates who were told ‘no.’ Why were they told no when they’re a good candidate? To say that it has nothing to do with reimbursement, I think, would be foolish.”
After receiving those types of comments, CMS wrote in its final decision that it is canceling its plan. “We recognize the importance of the patient-provider relationship and the practice of medicine in determining the most appropriate breast reconstruction procedure for each patient,” the agency wrote.
KFF Health News, formerly known as Kaiser Health News (KHN), is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling and journalism.
[ad_2]
Source link